BMJ:外科医生具体结果公开报告制度对结肠癌患者治疗方案及预后的影响
2018-05-04 zhangfan MedSci原创
研究认为外科医生具体结果公开报告制度对结肠癌手术患者治疗方法无显著影响,但患者术后死亡率呈下降趋势
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#BMJ#
21
#治疗方案#
0
学习了.谢谢分享
59
#外科医生#
25
了解一下.谢谢分享!
62
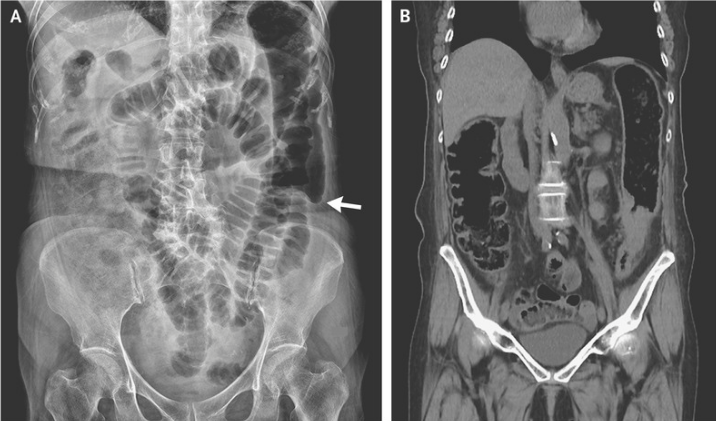
研究在英国开展.111431名结肠癌患者参与研究.主要考察患者择期结直肠癌手术后90天死亡率.研究主要终点为结直肠癌选择性大切除术患者的比例.根据病人和肿瘤特点预测90天的死亡率以及调整后患者90天死亡率.
66