BMJ子刊:胎龄小于26周的新生儿机械通气拔管成功的预测因素
2022-08-20 liangying MedSci原创
大多数胎龄(GA)小于26周的极早产(EP)婴儿需要接受机械通气(MV)。
大多数胎龄(GA)小于26周的极早产(EP)婴儿需要接受机械通气(MV)。虽然MV可以挽救生命,但呼吸机引起的肺损伤增加了慢性呼吸系统疾病的风险。因此,临床医生努力争取尽快拔管。然而,拔管失败很常见,原因与MV持续时间延长、住院时间延长以及医院感染和死亡风险增加有关。
EP婴儿理想拔管时机的临床评估是复杂的,包括确定最佳拔管前、拔管中和拔管后管理。因此,有必要开展有助于预测EP婴儿成功拔管的研究,本研究的目的是调查极早产(EP)婴儿的首次拔管尝试,并探讨可能提高拔管准备的临床判断质量的因素。
本研究为2013年1月1日至2018年12月31日期间在挪威进行,探索了26周胎龄(GA)前出生的EP婴儿的首次拔管尝试。通过挪威新生儿网络数据库确定了符合条件的婴儿。主要结果是成功拔管,定义为拔管后72小时内未再次插管。
在482名合格婴儿中,确定了316名首次拔管尝试的婴儿。总体而言,173名(55%)婴儿成功拔管,而143名(45%)婴儿第一次拔管失败。共有261名(83%)婴儿从常规通气(CV)拔管,55名(17%)婴儿从高频振荡通气(HFOV)拔管。从CV拔管时,拔管前吸入氧气的分数(FiO2)≤0.35、较高的Apgar评分、较高的GA、女性性别和较高的产后年龄是成功拔管的重要预测因素。从HFOV拔管时,拔管前的FiO2水平≤0.35是成功拔管的相关预测因子。
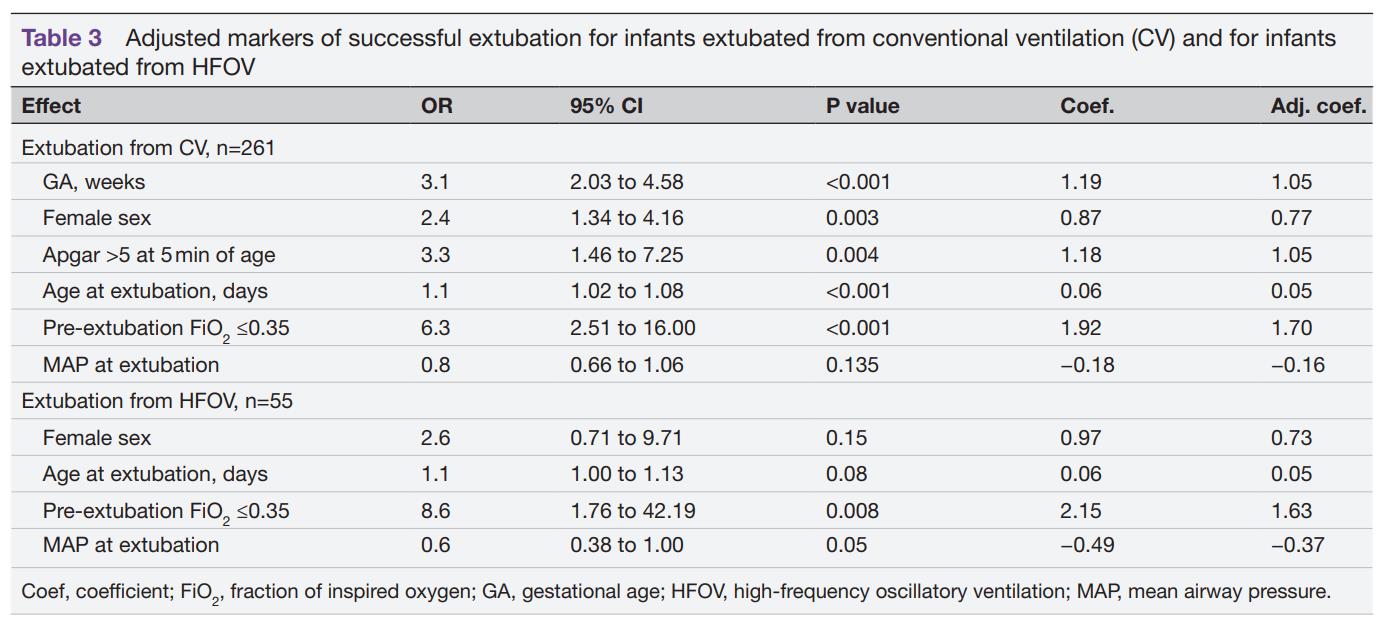
婴儿从常规通气(CV)和婴儿从HFOV拔管成功的标志
总之,正确的拔管时机对EP患儿非常重要。在这个国家队列研究中,55%的首次拔管尝试是成功的。当临床医生第一次给EP婴儿拔管时,额外注意氧气需求、性别和出生时的一般情况可能会进一步增加拔管成功率。
参考文献:
, et al Predictors of extubation success: a population-based study of neonates below a gestational age of 26 weeks
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#BMJ#
0
#胎龄#
46
学习学习
61
#预测因素#
54
#拔管#
40