十二指肠空肠交界区间质瘤致消化道大出血一例
2019-01-20 郭争荣 范小军 罗辉 中华消化内镜杂志
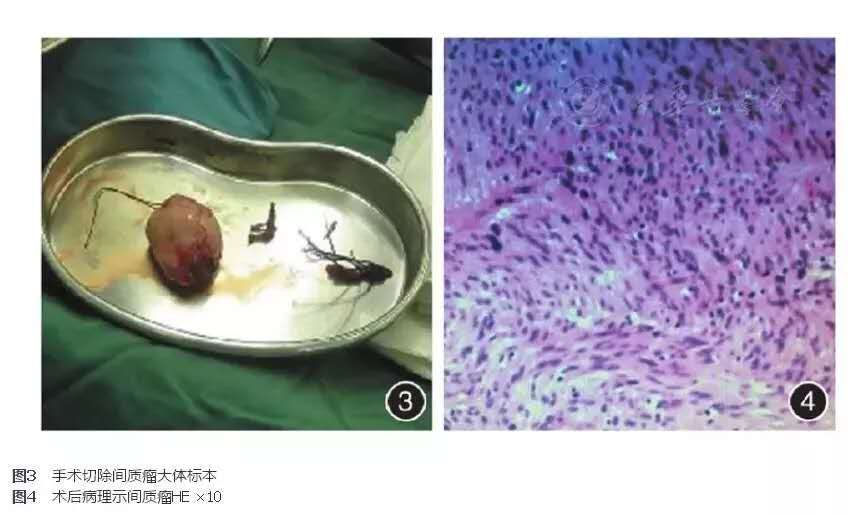
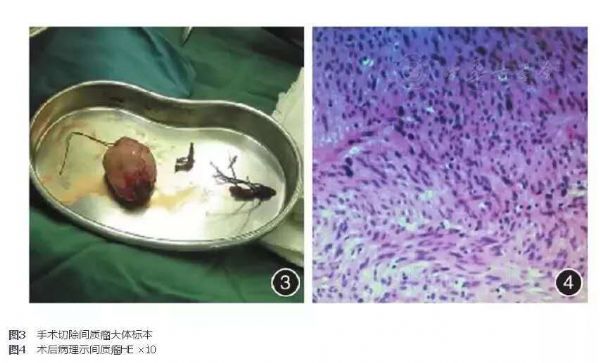
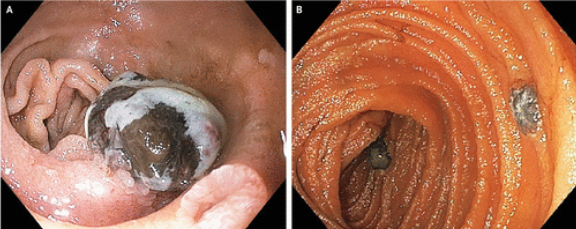
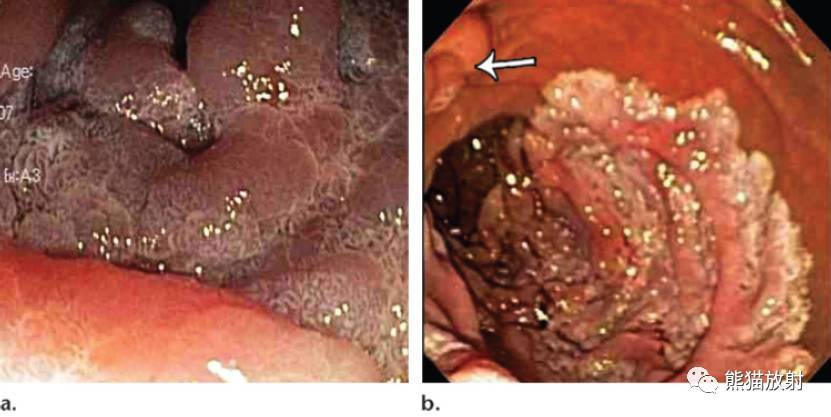
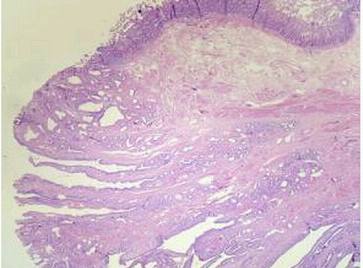
患者男,63岁,主因呕血、便血4d入院。患者4d前进正常食物后出现呕鲜红色血液及排暗红色血便3次,总量约1300mL,伴头晕、乏力,心慌、出汗等不适。就诊于我院急诊科,血常规示血红蛋白51g/L,急诊胃镜检查示十二指肠水平部可见大量鲜血,可见一小动脉持续性喷血,行内镜下钛夹止血(图1)。出血停止后收入普通病房。患者既往无消化道溃疡及肝病病史,无使用抗凝或抗血小板药物史,有高血压病史。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#十二指肠#
29
#消化道大出血#
40
#大出血#
29
#间质瘤#
26
#消化道#
28
好文,值得点赞!认真学习,应用于实践!谢谢分享给广大同好!
43