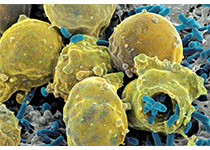
纤毛化的粘膜结节乳头状肿瘤是一种罕见的肺部肿瘤,迄今为止在英国文献中仅仅报道了38例。通常在老年人(平均年龄67岁)中偶然发现它是计算机断层扫描中的小的外围玻璃不透明或结节。在显微镜下,肿瘤由纤毛柱状,粘液和基底细胞的混合物组成,具有各种模式,包括腺体,乳头状,鳞片状和微毛细管生长模式。最近,研究表明肿瘤有几个相关的基因改变,支持病变确实是肿瘤性的。肿瘤似乎遵循惰性临床过程,因为没有报道复发或转移。在本文中,我们回顾了临床,影像学,病理学,和纤毛状多发性乳头状肿瘤的分子发现。讨论了诊断缺陷和诊断考虑因素。
原始出处:
Yen-Wen Lu and Yi-Chen Yeh, Ciliated
Muconodular Papillary Tumors of the Lung
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#乳头状#
25
#Pathol#
29
#结节性#
40
了解一下
37
#Med#
18