全麻术后恢复早期一过性失语一例
2019-07-17 张元贵 临床麻醉学杂志
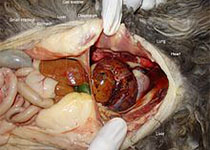
患者,女,30岁,166 cm,76kg,BMI 27.5kg/m2,ASAⅡ 级。急诊入院诊断:宫外孕,拟在全身麻醉下行“腹腔镜下宫外孕摘除术”。查体:HR 89次/分,RR 16次/分,BP108/60mmHg,体温36.6℃。术前检查示心、肺、肝肾功能和神经系统未见异常。既往体健,无精神疾病病史,无失语病史,未曾生育,自述两年前曾行宫外孕摘除术。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#一过性#
48
#失语#
46
#全麻术#
36
#全麻#
49